Content
Places to Stay Cool in Jax
Visit JaxReady.com for a map of city pools, splash pads, community centers and libraries where you can beat the heat with a splash of water or a blast of air conditioning.
Emergency Cooling Centers
Activation Thresholds
Emergency Cooling Centers will be activated under two maximum heat index thresholds:
- The National Weather Service (NWS) issues a Heat Advisory for Duval County for three or more consecutive days. The maximum heat index is expected to be between 108°F and 112°F.
- The National Weather Service (NWS) issues an Excessive Heat Warning for one or more days. The maximum heat index is expected to reach 113°F or higher.
Sunday & Holidays: For extreme heat events on Sundays and holidays, two main Emergency Cooling Centers will be specifically activated from 11:00 AM to 6:00 PM:
- Main Library (303 N. Laura St.)
- Legends Center (5130 Soutel Dr.)
Monday-Saturday: For extreme heat events on Mondays through Saturdays, Cooling Centers will be activated at various City of Jacksonville (COJ) facilities under normal hours of operation. These facilities will be open regardless of whether activation thresholds are met, and they include:
- All COJ Public Libraries (21 libraries). Accessible and air-conditioned spaces.
- All COJ Community Centers (20 centers). Available in multiple neighborhoods.
- All COJ Pools (29 pools) and Splash Pads (16 pads).
Visit JaxReady.com/StayCoolJax to find a cooling center location near you and for more information.
Transportation: Additionally, free transportation to Cooling Centers will be provided by the Jacksonville Transportation Authority (JTA) on designated Heat Emergency days. Residents must tell the bus driver that they are heading to or from a cooling center to receive free service. By offering free rides, JTA will help remove transportation barriers, allowing more community members to access the Cooling Centers, and in turn, stay cool and safe.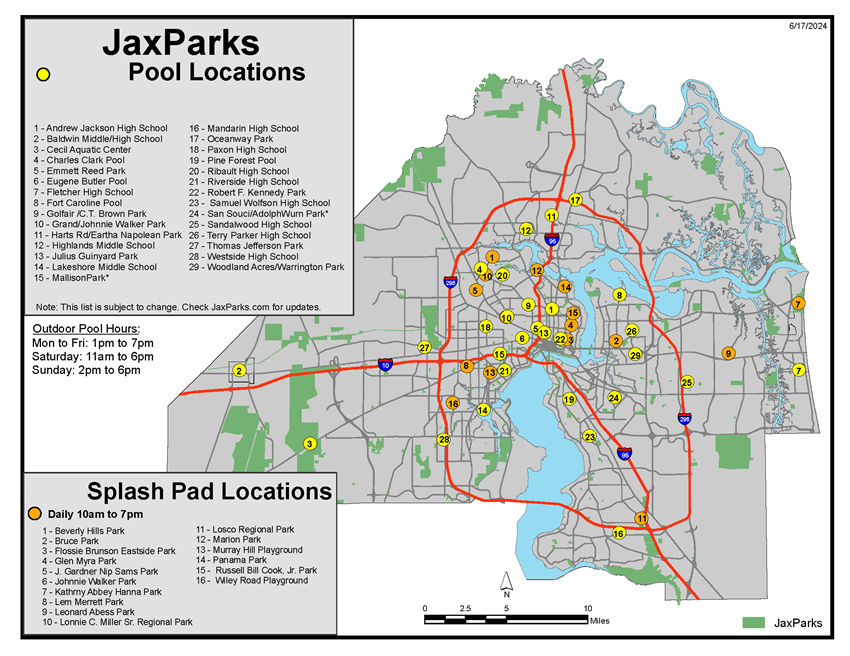
Children & Pet Heat Safety
Do Not Leave Children and Pets in a Vehicle: Never leave children or pets unattended in vehicles, as temperatures can quickly become dangerously high and potentially fatal. Idling the vehicle with air conditioning on and/or windows cracked is not effective at cooling your car’s interior. A young child’s or pet's body is not able to regulate its internal temperature like effectively. This causes the body temperature to rise 3 to 5 times faster than an adult, making them more vulnerable to severe outcomes such as heat stroke.
Tips for Children
- Avoid Peak Heat: Avoid Peak Heat: Minimize outdoor activities during the hottest part of the day, typically between 10 a.m. and 4 p.m. If you must be outside, find shade and take frequent breaks in cooler areas.
- Dress for the Weather: Wear lightweight, loose-fitting, and light-colored clothing to allow your skin to breathe. Opt for breathable fabrics such as cotton to help evaporate sweat and keep your body cool.
- Seek Air-Conditioned Environments: Spend time in air-conditioned places like malls, libraries, or community centers to escape the heat.
Tips for Pets
- Avoid dehydration: Pets can dehydrate quickly, so give them plenty of fresh, clean water.
- Don't leave your pet in a parked car: ON A WARM DAY, the temperature in a car can exceed 120° in a matter of minutes—even with the windows partially open. Your pet can quickly suffer brain damage or die from heatstroke or suffocation.
- Walk your dog in the morning and evening: When the temperature is very high, do not let your dog linger on hot asphalt or concrete. Your pet’s body can heat up quickly, and sensitive paw pads can burn.
- Know when your pet is in danger: Symptoms of overheating in pets include excessive panting or difficulty breathing, increased heart and respiratory rate, drooling, mild weakness, unresponsiveness, or even collapse.
Heat and its Effects on Health
What are heat cramps?
Heat cramps are the mildest form of heat illness and consist of painful muscle cramps and spasms that occur during or after intense exercise and sweating in high heat. Symptoms include:
- Painful cramps, especially in the legs
- Flushed, moist skin
What is heat exhaustion?
Heat exhaustion is more severe than heat cramps and results from a loss of water and salt in the body. It occurs in conditions of extreme heat and excessive sweating without adequate fluid and salt replacement. Heat exhaustion occurs when the body is unable to cool itself properly and, if left untreated, can progress to heat stroke.
- Muscle cramps
- Pale, moist skin
- Usually has a temp over 100.4° F (or 34° C)
- Nausea
|
- Vomiting
- Heavy Sweating
- Headache
|
- Fatigue
- Weakness
- Anxiety, and faint feeling
|
What is heat stroke?
Heat stroke, the most severe form of heat illness, occurs when the body's heat-regulating system is overwhelmed by excessive heat. It is a life-threatening emergency and requires immediate medical attention. Symptoms include:
- Warm, dry skin
- High fever, usually over 104° F (or 40° C)
- Rapid heart rate
- Loss of appetite
- Nausea
|
- Vomiting
- Headache
- Fatigue
- Confusion
|
- Agitation
- Lethargy
- Stupor
- Seizures, coma, and death are possible
|
Medical Conditions
If you have any of the following conditions, it’s important to be cautious during days with excessive heat warnings:
- Heart disease: Heat increases the risk of heart attacks, arrythmias and heart failure
- Asthma/COPD and any chronic lung disease
- Mental Health: More instances of suicide, homicide, violent crime on extremely hot days; Heat can exacerbate severity of symptoms in those with mood disorders and psychosis.
- Diabetes: With extremes in temperature, those with Diabetes (types 1 or 2) have a more difficult time regulating body temperature and blood glucose.
Medications
Medications can contribute to heat sensitivity by reducing the thirst sensation, interfering with mentation, decreasing perspiration, causing dehydration, low blood pressure and electrolyte imbalance.
Blood pressure medications
- Diuretics (such as furosemide, hydrochlorothiazide, acetazolamide) can lead to dehydration, electrolyte imbalance, increased risk of falling/fainting spells
- Beta Blockers (such as metoprolol, propranolol, atenolol) can lead to decreased sweating, reduced blood pressure, increased risk of falling/fainting spells
- Calcium Channel Blockers (such as amlodipine, nifedipine, felodipine) can lead to reduced blood pressure and increased risk of falling/fainting
- ACE inhibitors or ARBs (such as enalapril, lisinopril, ramipril, valsartan, losartan) decreased sense of thirst, reduced blood pressure, increased risk of falling/fainting
- Nitrates (such as nitroglycerin, isosorbide mononitrate) can lead to significant low blood pressure, increased risk of falling/fainting
Mental Health Medications
- Mood stabilizer (such as lithium) can lead to diabetes induced water loss and risk of fainting falls and electrolyte imbalance. There's also a risk of lithium toxicity associated with dehydration.
- Antipsychotics (such as haloperidol, risperidone, olanzapine) can lead to impaired perspiration which can increase body temperature
- Selective Serotonin Reuptake Inhibitors (such as fluoxetine, sertraline commonly known as Prozac and Zoloft) this can lead to increased sweating
- Stimulants (methylphenidate, dextroamphetamine commonly known as Ritalin and Adderall) can lead to increased body temperatures
- Tricyclic antidepressants (such as amitriptyline) can lead to decreased sweating
- Anti-seizure medications (carbamazepine, topiramate, ox carbamazepine) can lead to body temperature dysregulation, increased urination, dizziness, weakness.
- Older antihistamines (such as diphenhydramine commonly known as Benadryl) can lead to decreased sweating and impaired regulation of body temperature
- Over the counter pain medications (such as ibuprofen, aspirin, acetaminophen) can lead to kidney injury with dehydration, increased body temperatures, liver injury with dehydration
- Certain antibiotics (such as sulfonamides commonly known as Bactrim) can lead to kidney injury with dehydration
- Certain HIV medications (such as indinavir) can lead to kidney injury with dehydration
- Thyroid replacement (such as levothyroxine) can lead to impaired regulation of body temperature, constriction of blood vessels
Please remember that alcohol can lead to increased sweating, increased urination and impaired heat perception and is NOT considered as a way to hydrate.
Medications Damaged by the Heat
It is important to note that medications may be damaged with heat exposure as well. Commonly affected medications would include:
- Inhalers (used for asthma or COPD) that can actually burst in hot environments.
- Epinephrine auto injectors (commonly known as Epipen) may malfunction or deliver less epinephrine when in hot environments.
- Insulin should be stored in a refrigerator and may become less effective with prolonged heat exposure.
Medications and Skin Sensitivity When Exposed to the Sun
Some medications can increase the sensitivity of the skin to the sun:
- Antifungal medications (such as flucytosine, griseofulvin, and voriconazole)
- Certain Antibiotics (such as metronidazole, tetracyclines and fluoroquinolones commonly known as Flagyl, Doxycycline, Cipro, Levaquin) can increase sun sensitivity and lead to a sunburn-like rash.
For patients on these medications, sun avoidance, protective clothing and hats, and broad-spectrum sunscreen that filters out UVA and UVB rays, with an SPF of 30 or higher, are recommended.